Pulmonary hypertension
Pulmonary hypertension or pulmonary arterial hypertension is a condition where there is high blood pressure in the lungs. Most people call it pah, ph or pha.
| Pulmonary hypertension | |
|---|---|
| Other names | Pulmonary arterial hypertension,[1] Ayerza syndrome[2] |
 | |
| Pulmonary hypertension | |
| Medical specialty | Pulmonology, cardiology |
| Symptoms | Chest pain, fatigue[3] |
| Usual onset | 20 to 60 years old[4] |
| Duration | Long term[1] |
| Causes | Unknown[1] |
| Risk factors | Family history, pulmonary embolism, HIV/AIDS, sickle cell disease, cocaine use, COPD, sleep apnea, living at high altitudes[5][4] |
| Diagnostic method | Following ruling out other potential causes[1] |
| Treatment | Supportive care, various medications, lung transplantation[1][6] |
| Medication | Epoprostenol, treprostinil, iloprost, bosentan, ambrisentan, macitentan, sildenafil[1] |
| Frequency | 1,000 new cases a year (US)[2] |
This condition makes it hard to breathe. Some people with the condition need extra oxygen (oxygen therapy). This condition can also make a person dizzy and become easily tired. Some people with the condition faint easily. The symptoms get worse when exercising or working hard. Pulmonary hypertension is a serious condition, and it can be fatal. The condition makes it harder for the heart to pump blood. Because the heart has to work harder, it can also become sick. Some people who are very sick may need a lung transplant or a heart-lung transplant to live.
Signs and symptoms
changePeople with pulmonary hypertension have difficulty breathing. Other signs and symptoms may be present. They may tire easily. Some may also faint more easily. There might be chest pain. Some patients have swelling of the feet and ankles (edema). These symptoms get worse during exercise or hard work.
Because many diseases can make it hard to breathe, a doctor must learn about the patient's background and do tests. This helps the doctor to treat the patient or find the right cause of the symptoms. Pulmonary hypertension makes the heart sound different. One test is to measure the blood pressure inside the pulmonary artery, the blood vessel that goes from the heart to the lungs.
In order to establish the cause, the physician will conduct a thorough medical history. A detailed family history is taken to determine whether the disease might be genetic. A history of drugs such cocaine, methamphetamine, alcohol, leading to cirrhosis, and smoking leading to emphysema are considered significant. Physical examination is performed to look for typical signs of pulmonary hypertension including a loud P2 (pulmonic valve closure sound), (para)sternal heave, jugular venous distension, pedal edema, ascites, hepatojugular reflux, clubbing etc.
Effects
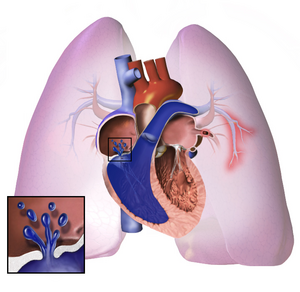
changeIn pulmonary hypertension, the blood vessels in the lungs become too narrow. The blood pressure in the lungs becomes high. The heart works very hard to pump blood through the narrow blood vessels. Later on, the blood vessels in the lungs become hard and thick. The heart must work harder.
The heart can work so hard that it becomes sick. This is called heart failure. The sick heart cannot pump blood well. Less blood goes to the lungs, so the blood gets less oxygen. This makes it hard to breathe. This may get worse with exercise.
Causes
changeThe most common cause of pulmonary hypertension is left heart failure. This causes pulmonary venous hypertension. This leads to pulmonary edema, or fluid build-up in the lungs.
Many illnesses can cause pulmonary arterial hypertension (PAH).
- Lung diseases that make the blood have less oxygen, such as:
- immune system problems, such as:
- AIDS
- scleroderma
- other autoimmune disorders
- liver problems
- other causes
- sleep apnea
- taking pills to lose weight, such as Fen-Phen, Aminorex, fenfluramine (Pondimin), and phentermine[7]
- sickle cell disease,[8]
- congenital heart disease
- thyroid diseases,[9]
- taking drugs like cocaine
- possibly Human herpesvirus 8[10]
When a person has pulmonary hypertension without any other cause, this is called idiopathic pulmonary arterial hypertension or IPAH.
When a family history exists, the disease is termed familial pulmonary arterial hypertension, (FPAH). IPAH and FPAH are now considered to be genetic disorders linked to mutations in the BMPR2 gene, which encodes a receptor for bone morphogenetic proteins,[11] as well as the 5-HT(2B) gene, which codes for a serotonin receptor.[12]
In medicine, pulmonary hypertension (PH) is an increase in blood pressure in the pulmonary artery or lung vasculature, leading to shortness of breath, dizziness, fainting, and other symptoms, all of which are made worse (exacerbated) by exertion. Depending on the cause, pulmonary hypertension can be a severe disease with a markedly decreased exercise tolerance and right-sided heart failure. It was first identified by Dr Ernst von Romberg in 1891.[13] It can be one of five different types, arterial, venous, hypoxic, thromboembolic, or miscellaneous.
Although the terms primary pulmonary hypertension, and secondary pulmonary hypertension (meaning due to another medical condition) still persist in materials disseminated to patients and the general public, these terms have largely been abandoned in the medical literature. This change has occurred because the older dichotomous classification did not reflect pathophysiology or outcome. It led to erroneous therapeutic decisions, i.e. treat "primary" pulmonary hypertension only. This in turn led to therapeutic nihilism for many patients labeled "secondary" pulmonary hypertension, and could have contributed to their deaths. The term "primary pulmonary hypertension" has now been replaced with "idiopathic pulmonary arterial hypertension". The terms "primary" and "secondary" pulmonary hypertension should not be used any longer. Further details are in the Classification section below.
Causes
changeThe most common cause of pulmonary hypertension is left heart failure leading to pulmonary venous hypertension. This may be due to systolic or diastolic malfunction of the left ventricle or due to valvular dysfunction such as mitral regurgitation or mitral stenosis. It usually manifests as pulmonary edema.
Common causes of pulmonary arterial hypertension (PAH) include HIV, scleroderma and other autoimmune disorders, cirrhosis and portal hypertension, sickle cell disease,[8] congenital heart disease, thyroid diseases,[9] and others. Use of weight loss pills such as Fen-Phen, Aminorex, fenfluramine (Pondimin), and phentermine led to the development of PAH in the past.[7]
Pathogenesis
changeWhatever the initial cause, pulmonary hypertension involves the tightening of blood vessels connected to and within the lungs. This makes it harder for the heart to pump blood through the lungs, much as it is harder to make water flow through a narrow pipe as opposed to a wide one. Over time, the affected blood vessels become both stiffer and thicker, further increasing the blood pressure within the lungs and impairing blood flow. In addition, the increased workload of the heart causes thickening and enlargement of the right ventricle, making the heart less able to pump blood through the lungs, causing right heart failure. As the blood flowing through the lungs decreases, the left side of the heart receives less blood. This blood may also carry less oxygen than normal. Therefore, it becomes harder and harder for the left side of the heart to pump to supply sufficient oxygen to the rest of the body, especially during physical activity.
Diagnosis
changeBecause pulmonary hypertension can be of 5 major types, a series of tests must be performed to distinguish pulmonary arterial hypertension from venous, hypoxic, thomboembolic, or miscellaneous varieties.
A physical examination is performed to look for typical signs of pulmonary hypertension. These include altered heart sounds, such as a widely split S2 or second heart sound, a loud P2 or pulmonic valve closure sound (part of the second heart sound), (para)sternal heave, possible S3 or third heart sound, and pulmonary regurgitation. Other signs include jugular venous distension (enlargement of the jugular veins), peripheral edema (swelling of the ankles and feet), ascites (abdominal swelling due to the accumulation of fluid), hepatojugular reflux, and clubbing.
Further procedures are required to confirm the presence of pulmonary hypertension and exclude other possible diagnoses. These generally include pulmonary function tests, blood tests, electrocardiography (ECG), arterial blood gas measurements, X-rays of the chest (followed by high-resolution CT scanning if interstitial lung disease is suspected), and ventilation-perfusion or V/Q scanning to exclude chronic thromboembolic pulmonary hypertension. Biopsy of the lung is usually not indicated unless the pulmonary hypertension is thought to be due to an underlying interstitial lung disease. But lung biopsies are fraught with risks of bleeding due to the high intrapulmonary blood pressure. Clinical improvement is often measured by a "six-minute walk test", i.e. the distance a patient can walk in six minutes. Stability and improvement in this measurement correlate with better survival.
Although pulmonary arterial pressure can be estimated on the basis of echocardiography, pressure sampling with a Swan-Ganz catheter provides the most definite measurement. PAOP and PVR can not be measured directly with echocardiography. Therefore, diagnosis of PAH requires a cardiac catheterization. A Swan-Ganz catheter can also measure the cardiac output, which is far more important in measuring disease severity than the pulmonary arterial pressure.
Normal pulmonary arterial pressure in a person living at sea level has a mean value of 12–16mmHg (1600–2100 Pa). Definite pulmonary hypertension is present when mean pressures at rest exceed 25mmHg (3300 Pa). If mean pulmonary artery pressure rises above 30mmHg (4000Pa) with exercise, that is also considered pulmonary hypertension.
Diagnosis of PAH requires the presence of pulmonary hypertension with two other conditions. Pulmonary artery occlusion pressure (PAOP or PCWP) must be less than 15mmHg (2000 Pa) and pulmonary vascular resistance (PVR) must be greater than 3 Wood units (240 dyn•s•cm−5 or 2.4mN•s•cm−5).
Classification
changeCurrent classification
changeIn 2003, the 3rd World Symposium on Pulmonary Arterial Hypertension was convened in Venice to modify the classification based on the new understanding of disease mechanisms. The revised system developed by this group provides the current framework for understanding pulmonary hypertension.
The system includes several improvements over the former 1998 Evian Classification system. Risk factor descriptions were updated, and the classification of congenital systemic-to pulmonary shunts was revised. A new classification of genetic factors in PH was recommended, but not implemented because available data were judged to be inadequate.
The Venice 2003 Revised Classification system can be summarized as follows:[14]
- WHO Group I - Pulmonary arterial hypertension (PAH)
- WHO Group II - Pulmonary hypertension associated with left heart disease
- WHO Group III - Pulmonary hypertension associated with lung diseases and/or hypoxemia
- WHO Group IV - Pulmonary hypertension due to chronic thrombotic and/or embolic disease
- WHO Group V - Miscellaneous
Previous terminology
changeThe terms primary and secondary pulmonary hypertension (PPH and SPH) were formerly used to classify the disease. This led to the assumption that only the primary disease should be treated, and the secondary variety should be ignored in favor of treating only the underlying illness. In fact all forms of pulmonary arterial hypertension are treatable. Unfortunately, this classification system still persists in the minds of many physicians, and probably leads to many patients with being denied treatment. This nihilistic approach to pulmonary arterial hypertension may also contribute to underdiagnosis. It is estimated that there are about 100,000 patients with PAH in the US, but only 15-20,000 have been diagnosed. Many others have been misdiagnosed as COPD, asthma, or congestive heart failure.
The term primary pulmonary hypertension (PPH) has now been replaced with idiopathic pulmonary arterial hypertension (IPAH) in much of the medical literature. However, some physicians continue to use the older classification inappropriately.
Epidemiology
changeIPAH is a rare disease with an incidence of about 2-3 per million per year and a prevalence of about 15 per million. Women are almost three times as likely to present with IPAH than men.
Other forms of PAH are far more common. In scleroderma the incidence has been estimated to be 6 to 60% of all patients, in rheumatoid arthritis up to 21%, in systemic lupus erythematosus 4 to 14%, in portal hypertension between 2 and 5%, in HIV about 0.5%, and in sickle cell disease ranging from 20 to 40%.
Diet pills such as Fen-Phen produced an annual incidence of 25-50 per million per year.
Treatment
changeTreatment is determined by whether the PH is arterial, venous, hypoxic, thromboembolic, or miscellaneous. Since pulmonary venous hypertension is synonymous with congestive heart failure, the treatment is to optimize left ventricular function by the use of diuretics, beta blockers, ACE inhibitors, etc., or to repair/replace the mitral valve or aortic valve.
In PAH, lifestyle changes, digoxin, diuretics, oral anticoagulants, and oxygen therapy are considered conventional therapy, but have never been proven to be beneficial in a randomized, prospective manner.
High dose calcium channel blockers are useful in only 5% of IPAH patients who are vasoreactive by Swan-Ganz catheter. Unfortunately, calcium channel blockers have been largely misused, being prescribed to many patients with non-vasoreactive PAH, leading to excess morbidity and mortality.
Vasoactive substances
changeThree major pathways are involved in abnormal proliferation and contraction of the smooth-muscle cells of the pulmonary artery in patients with pulmonary arterial hypertension. These pathways correspond to important therapeutic targets in this condition and play a role in determining which of three classes of drugs—endothelin receptor antagonists, phosphodiesterase type 5 inhibitors, and prostacyclin derivatives—will be used.
Prostacyclin (prostaglandin I2) is commonly considered the most effective treatment for PAH. Epoprostenol (synthetic prostacyclin, marketed as Flolan®) is given via continuous infusion that requires a semi-permanent central venous catheter. This delivery system can cause sepsis and thrombosis. Flolan® is unstable, and therefore has to be kept on ice during administration. Since it has a half-life of 3 to 5 minutes, the infusion has to be continuous (24/7), and interruption can be fatal. Other prostanoids have therefore been developed. Treprostinil (Remodulin®) can be given intravenously or subcutaneously, but the subcutaneous form can be very painful. Iloprost (Ilomedin®) is also used in Europe intravenously and has a longer half life. Iloprost (marketed as Ventavis®) is the only inhaled form of prostacyclin approved for use in the US and Europe. This form of administration has the advantage of selective deposition in the lungs with less systemic side effects.
The dual (ETA and ETB) endothelin receptor antagonist bosentan (marketed as Tracleer®) was approved in 2001. Two selective endothelin receptor antagonists (ETA only) are in the final stages of approval: sitaxsentan and ambrisentan. Sildenafil, a selective inhibitor of cGMP specific phosphodiesterase type 5 (PDE5), was approved for the treatment of PAH in 2005. It is marketed for PAH as Revatio®. Tadalafil (currently marketed as Cialis® for erectile dysfunction) is currently is Phase III trials. Vasoactive intestinal peptide by inhalation should enter clinical trials for PAH in 2007. PRX-08066 is a serotonin antagonist currently being developed for hypoxic pulmonary hypertension.
Surgical
changeAtrial septostomy is a surgical procedure that creates a communication between the right and left atria. It relieves pressure on the right side of the heart, but at the cost of lower oxygen levels in blood (hypoxia). It is best performed in experienced centers. Lung transplantation cures pulmonary arterial hypertension, but leaves the patient with the complications of transplantation, and a survival of about 5 years.
Pulmonary thromboendarterectomy (PTE) is a surgical procedure that is used for chronic thromboembolic pulmonary hypertension. It is the surgical removal of an organized thrombus (clot) along with the lining of the pulmonary artery; it is a large and very difficult procedure that is currently performed in a few select centers. Case series show remarkable success in most patients.
Treatment for hypoxic and miscellaneous varieties of pulmonary hypertension have not been established. However, studies of several agents are currently enrolling patients. Many physicians will treat these diseases with the same medications as for PAH, until better options become available.
Prognosis
changeThe NIH IPAH registry from the 1980s showed an untreated median survival of 2–3 years from time of diagnosis, with the cause of death usually being right ventricular failure (cor pulmonale). Although this figure is widely quoted, it is probably irrelevant today. Outcomes have changed dramatically over the last two decades. This is because of newer drug therapy, better overall care, and earlier diagnosis (lead time bias). A recent outcome study of those patients who had started treatment with bosentan (Tracleer®) showed that 86% patients were alive at 3 years. With multiple agents now available, combination therapy is increasingly used. Impact of these agents on survival is not known, since many of them have been developed only recently. It would not be unreasonable to expect median survival to extend past 10 years in the near future.
References
change- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Cite error: The named reference
NORD2015was used but no text was provided for refs named (see the help page). - ↑ 2.0 2.1 Cite error: The named reference
GHR2016was used but no text was provided for refs named (see the help page). - ↑ Cite error: The named reference
webwas used but no text was provided for refs named (see the help page). - ↑ 4.0 4.1 Cite error: The named reference
NIH2011Riskwas used but no text was provided for refs named (see the help page). - ↑ Cite error: The named reference
NIH2011Cawas used but no text was provided for refs named (see the help page). - ↑ Cite error: The named reference
NIH2011Txwas used but no text was provided for refs named (see the help page). - ↑ 7.0 7.1 Abenhaim L, Moride Y, Brenot F, Rich S, Benichou J, Kurz X, Higenbottam T, Oakley C, Wouters E, Aubier M, Simonneau G, Begaud B. Appetite-suppressant drugs and the risk of primary pulmonary hypertension. International Primary Pulmonary Hypertension Study Group. N Engl J Med 1996;335:609-16. PMID 8692238.
- ↑ 8.0 8.1 Gladwin MT, Sachdev V, Jison ML, Shizukuda Y, Plehn JF, Minter K, Brown B, Coles WA, Nichols JS, Ernst I, Hunter LA, Blackwelder WC, Schechter AN, Rodgers GP, Castro O, Ognibene FP. Pulmonary hypertension as a risk factor for death in patients with sickle cell disease. N Engl J Med 2004;350:886-95. PMID 14985486.
- ↑ 9.0 9.1 Curnock AL, Dweik RA, Higgins BH, Saadi HF, Arroliga AC. High prevalence of hypothyroidism in patients with primary pulmonary hypertension. Am J Med Sci 1999;318:289-292. PMID 10555089.
- ↑ Cool CD, Rai PR, Yeager ME, Hernandez-Saavedra D, Serls AE, Bull TM, Geraci MW, Brown KK, Routes JM, Tuder RM, Voelkel NF. Expression of Human Herpesvirus 8 in Primary Pulmonary Hypertension.N Engl J Med 2003;349:1113-22. PMID 13679525.
- ↑ Deng Z, Morse JH, Slager SL, Cuervo N, Moore KJ, Venetos G, Kalachikov S, Cayanis E, Fischer SG, Barst RJ, Hodge SE, Knowles JA. Familial primary pulmonary hypertension (gene PPH1) is caused by mutations in the bone morphogenetic protein receptor-II gene. Am J Hum Genet 2000;67:737-44. PMID 10903931.
- ↑ Blanpain C, Le Poul E, Parma J, Knoop C, Detheux M, Parmentier M, Vassart G, Abramowicz MJ. Serotonin 5-HT(2B) receptor loss of function mutation in a patient with fenfluramine-associated primary pulmonary hypertension. Cardiovasc Res 2003;60(3):518-28. PMID 14659797.
- ↑ Romberg E von. Über Sklerose der Lungenarterie. Dtsch Arch Klin Med 1891-1892;48:197-206.
- ↑ Proceedings of the 3rd World Symposium on Pulmonary Arterial Hypertension. Venice, Italy, June 23-25, 2003. J Am Coll Cardiol 2004 Jun 16;43(12 Suppl S):1S-90S. PMID 15194171.
Other websites
change- The Merck Manual of Diagnosis and Therapy: Pulmonary Hypertension
- PH Central - the internet resource for Pulmonary Arterial Hypertension
- The Pulmonary Hypertension Association Webpage provided by the Pulmonary Hypertension Association
- Facts About Primary Pulmonary Hypertension from the National Heart, Lung, and Blood Institute (NHLBI)
- Webcast: The Changing World of Pulmonary Arterial Hypertension Therapies - American College of CHEST Physicians Archived 2006-10-17 at the Wayback Machine
- Pulmonary Arterial Hypertension Information for Healthcare professionals
- BMPR2-Related Primary Pulmonary Hypertension on GeneReviews[permanent dead link]
- "Cialis at Pharmacists.org (Generic Name: Tadalafil)". May 2023.